How to Increase Progesterone Naturally
Low progesterone is a common concern after pregnancy or infant loss, especially for women preparing to conceive again. This article explains how progesterone supports recovery and fertility, how to assess levels accurately, and how to raise progesterone naturally.
Caroline Bomer
1/5/20267 min read
Low progesterone is one of the most common hormonal concerns I see in women after pregnancy or infant loss, especially in women who want to support their recovery so they can feel confident as they try to conceive again.
Progesterone plays a major role in regulating your cycle, improving implantation, and maintaining a healthy pregnancy. Yet it’s often overlooked, poorly tested, or misunderstood.
In this article, we’ll walk through what low progesterone can look like, how to accurately check progesterone levels, and how to raise progesterone naturally in a way that supports recovery and future fertility.
NOTE: If you’re worried that low progesterone caused a previous loss, do not blame yourself. You could not have known, and it is not your fault. Many women are never told this is even a factor in fertility, which is why I wrote this. Instead of guilt, use this as an invitation to be better educated, prepared, and reassured as you move forward.
Why Progesterone Matters for Recovery and Future Fertility
Progesterone is responsible for implantation, calming your mood, balancing estrogen, increasing your metabolism and appetite, supporting clearer decision making, and supporting pregnancy.
That’s literally how it got its name: pro + gestation, meaning “for pregnancy.”
After loss, progesterone is a key part of how the body repairs, stabilizes, and finds rhythm again. Supporting healthy progesterone levels is not about forcing your body forward, but about giving it what it needs to rebuild and prepare.
How to Accurately Check Your Progesterone Levels
When it comes to checking hormones, most women assume the first step is going to their doctor or midwife for blood work. While labs can be helpful, there are a few important things to understand first.
This article is for educational purposes and is not a substitute for individualized medical care.
Blood Work
If you choose to test progesterone through blood work, timing is everything.
Hormones don’t just change from phase to phase. They fluctuate day to day and even throughout the day. Progesterone does not rise evenly like a steady stream, but instead is released in bursts throughout the day during the Luteal phase.
Because of this, testing at the wrong time can easily make progesterone appear lower than it actually is.
You’ll often see recommendations online to test progesterone on Day 21-22 of your cycle. This advice assumes:
You ovulate on Day 14
Your luteal phase is a standard length
For most women, neither of those assumptions is true. This is why, as we’ll talk about later, cycle charting is key.
Another important consideration is interpretation. There is a big difference between “normal” progesterone levels and optimal levels. While some reference ranges list normal progesterone as anywhere from about 1.8–20 ng/mL, optimal levels for fertility and hormonal balance are closer to 15 ng/mL during the luteal phase. That's a significant difference.
Getting the timing right and properly interpreting results is essential.
Other Tests to Consider
Blood work is just one piece of the puzzle.
D.U.T.C.H. TESTING
The DUTCH test (Dried Urine Test for Comprehensive Hormones) looks not only at how much hormone is present, but how your body produces, uses, and eliminates hormones.
This can be especially helpful if:
You suspect progesterone is low
Estrogen may be overpowering progesterone
Stress is causing progesterone to be converted into cortisol
The downside is that this test is often not covered by insurance, and not all practitioners are well-trained in interpreting the results. Still, it can be a very valuable tool when used appropriately.
HTMA (Hair Tissue Mineral Analysis)
HTMA looks at your mineral status over the last 3 months using a small hair sample, giving you a wide photo instead of a snapshot of a singular moment like blood tests do. While it doesn’t measure progesterone directly, it helps identify whether you have the building blocks needed for hormone production (like zinc) as well as patterns related to stress and thyroid health.
Nothing in the body works in isolation. If progesterone is low, it’s often connected to other systems that need support. HTMA gives more context with a big picture of the bedrock of your overall health- your minerals.
Cycle Charting: The Easiest Way to Check Progesterone
One of the simplest and most effective ways to assess progesterone is to chart your cycle.
If you are not ovulating, you are not making progesterone. No test required.
Ovulation is what allows the ovarian follicle (the sac that releases an egg) to transform into a temporary organ called the corpus luteum. This is what produces progesterone throughout the luteal phase. If ovulation doesn’t occur, that organ never develops, meaning progesterone isn’t produced for that cycle.
How to Confirm Ovulation
Despite what TV shows suggest, a high temperature does not mean you are currently ovulating. Progesterone raises your temperature after ovulation, once the egg has been released and the corpus luteum begins producing hormones.
The only cycle charting method that confirms ovulation is with BBT (Basal Body Temperature)- all others only help predict it.
This is your baseline temperature taken as soon as you wake up after 3-4 hours of uninterrupted sleep. "Basal" simply means it's more precise, going to the hundredth decimal point (i.e. 97.34 °F instead of 97.3 °F).
Luteal Phase Length Matters
After confirming ovulation, the next step is tracking the length of your luteal phase.
Ideally, it is 12 days or longer, though 10+ days is still a good place to be. A short luteal phase can indicate insufficient progesterone to maintain the uterine lining, often showing up as:
Spotting
Early periods
Brown menstrual blood
Difficulty sustaining a pregnancy
These are the first two things I look at with anyone concerned about conceiving or hormonal recovery because they clearly show where support is most needed.
Cycle Charting Cheat Sheet
This is why I emphasize cycle charting so heavily when working with women preparing to conceive. Knowing how to read your body’s signals allows you to spot potential risks early and support them proactively.
With the Cycle Charting Cheat Sheet, you can track:
BBT
Cervical mucus
Phase lengths
Luteal phase trends
Charting provides clarity. Personalized guidance helps you know what to do with that information, especially when preparing to try to conceive again. If you want to understand your chart, hormones, and symptoms, and a clear plan to help your recovery, click here to learn more about working with me 1:1.
Signs of Low Progesterone
Other common signs of low progesterone include:
→ Luteal phase shorter than 10 days
→ Anovulatory cycles (a period without ovulation)
→ Irregular cycles
→ Missing periods
→ PMS and mood swings
→ Spotting
→ Poor sleep during the luteal phase
→ Difficulty conceiving
→ Difficulty staying pregnant
→ Anxiety
How to Raise Progesterone Naturally
Before trying to raise progesterone, it’s important to confirm that ovulation is occurring. If it isn’t, that becomes the starting point.
If ovulation is happening but progesterone is still low, here’s where to focus.
Not sure which of these areas is most relevant for your body and recovery? This is something I help clients identify quickly in 1:1 work. Read more →
Nutrition
It’s hard to create something out of nothing. If your body doesn’t have the nutrients it needs, it cannot make progesterone.
Key nutrients include:
✓ Cholesterol & Saturated Fats
All hormones are made from cholesterol. About 80% of cholesterol is produced internally by the liver using saturated fats, primarily from animal foods and some plant sources like coconut oil.
✓ Pre-Formed Vitamin A
Pre-formed vitamin A- only found in animal foods- is required to convert cholesterol into pregnenolone, which later becomes progesterone. Liver is the one of the best sources by far. Try adding a scoop of dessicated liver to any dish with ground beef and sauce to get the big impact without the big taste. Or try taking it as a pill.
Perfect Supplements Beef Liver - use the code FLOURISHNFLOW for an extra 10% off your entire order.
✓ Vitamin B3 (Niacin)
Supports the enzyme that converts pregnenolone into progesterone. Found in tuna, beef liver, chicken breast, and salmon.
✓ Vitamin B6
Supports estrogen breakdown in the liver and has been shown to help lengthen the luteal phase. Found in salmon, chicken, and sweet potatoes.
✓ Zinc
Important for follicle development before ovulation, which later impacts progesterone production. Found in oysters, beef, bison, and pumpkin seeds.
✓ Vitamin C (Whole-Food Sources)
Whole-food vitamin C during the luteal phase has been shown to significantly increase progesterone levels. Ascorbic Acid- found in most products- is synthetic and is used differently by the body than whole-food sources. Fresh fruit is the best source. Since it's the vitamin most sensitive to oxidation, you'll get more the fresher your food is. For an added boost, add acerola cherry powder to your drinks or smoothies and get 267% of your daily value in just 1/4 tsp!
Perfect Supplements Acerola Cherry - use code FLOURISHNFLOW for 10% your entire order
Bonus: During the luteal phase, progesterone increases metabolism, meaning you may need about 10% more calories. Undereating during this phase can increase stress hormones and suppress progesterone.
Stress and Hormone Conversion
Stress affects progesterone in two main ways:
By preventing ovulation
By converting progesterone into cortisol
Remember, if you don't ovulate, you literally cannot make progesterone. But it doesn't stop there- when stressed, your body converts progesterone into cortisol. This is protective. It simultaneously puts reproduction on the backburner while driving attention to deal with the immediate stressor. It's possible that you're producing enough progesterone, but too stressed to keep it.
Stress isn't just mental. It also includes:
Undereating
Blood sugar instability
Inadequate minerals
High energy demands
Over-exercising
Supporting progesterone means supporting your body’s ability to meet its energy needs so it doesn’t have to choose survival hormones over reproductive ones.
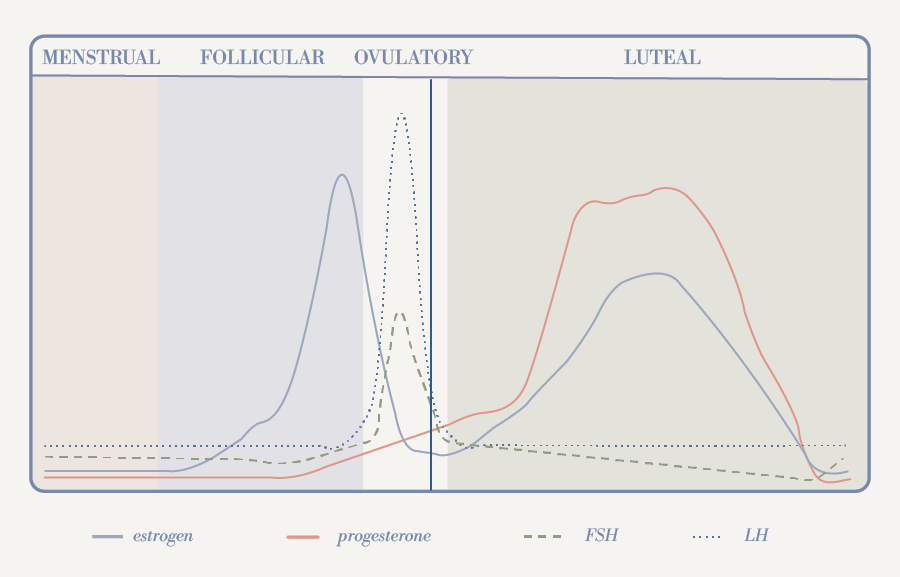
Estrogen Balance
Estrogen and progesterone are complementary- as one rises, the other decreases. It's a beautiful dance of balance and harmony. Many women experience estrogen dominance, where estrogen is high relative to progesterone.
This can be influenced by:
High stress
Synthetic hormones
Endocrine disruptors
Impaired gut or liver elimination
Supporting estrogen balance includes:
Increasing fiber intake (especially raw carrots)
Reducing toxic load from everyday products
Supporting gut and liver health
Healthy progesterone depends on healthy estrogen balance.
Final Thoughts
There is a lot that goes into progesterone production, but it ultimately comes back to supporting the basics: ovulation, nourishment, energy, and balance.
If you suspect you have low progesterone and want guidance on where to start, this is exactly the work I do with my 1:1 clients. Together, we look at your cycle, symptoms, and lifestyle to create a clear plan forward.
→ Learn more about 1:1 support
Healthy progesterone levels are key to feeling confident in your recovery and your future fertility. And now you’re one step closer.